Per diem nursing positions offer a unique blend of flexibility, variety, and financial incentives that appeal to many healthcare professionals. Whether you’re a seasoned nurse seeking a change or a nursing student exploring career options, understanding the advantages of per diem roles can help you make informed decisions about your professional path. Understanding Per Diem Nursing Per diem, meaning “per day,” refers to nursing positions where professionals work on an as-needed basis, filling in for staff shortages, covering peak periods, or providing additional support during high-demand times. Unlike full-time roles, per diem nurses have the autonomy to choose their shifts and work locations, offering a level of flexibility not typically found in traditional nursing positions. Key Benefits of Per Diem Nursing Positions 1. Flexible Scheduling One of the most significant advantages of per diem nursing is the ability to control your work schedule. This flexibility allows nurses to: This autonomy can lead to improved work-life balance and reduced burnout. 2. Higher Hourly Compensation Per diem nurses often receive higher hourly wages compared to their full-time counterparts. This increased pay compensates for the lack of benefits and job security associated with full-time positions. Additionally, working during weekends, holidays, or night shifts can further boost earnings due to shift differentials. 3. Diverse Work Environments Working per diem allows nurses to gain experience in various healthcare settings, including: This exposure enhances clinical skills, adaptability, and can inform future career decisions. 4. Opportunities for Skill Development Per diem roles provide the chance to work across different specialties and patient populations, fostering continuous learning and professional growth. Nurses can acquire new competencies and stay updated with the latest healthcare practices. 5. Networking and Career Advancement Engaging with various healthcare teams and institutions expands professional networks. These connections can lead to future job opportunities, references, and collaborations, enhancing career prospects. 6. Supplemental Income For nurses with existing full-time positions, per diem work offers a means to earn additional income. This extra financial resource can be allocated towards savings, education, or other personal goals. 7. Reduced Workplace Politics Per diem nurses often have limited involvement in internal administrative matters, allowing them to focus primarily on patient care. This detachment can lead to a more straightforward and less stressful work experience. Considerations Before Pursuing Per Diem Nursing While per diem positions offer numerous benefits, it’s essential to be aware of potential challenges: Assessing personal circumstances and career goals is crucial when considering per diem nursing. Is Per Diem Nursing Right for You? Per diem nursing may be a suitable option if you: Finding Per Diem Nursing Opportunities To explore per diem nursing positions: Researching and selecting the right opportunities can lead to a fulfilling per diem nursing experience. Conclusion Per diem nursing positions offer a compelling alternative to traditional full-time roles, providing flexibility, diverse experiences, and financial benefits. By understanding the advantages and considerations, nurses can make informed decisions that align with their personal and professional aspirations. If you’re interested in exploring per diem nursing opportunities, contact our team to learn more about available positions and how we can assist you in achieving your career goals.
Author: Blessings Osayomore
How to Land High-Paying Travel Nursing Jobs and Top Specialties
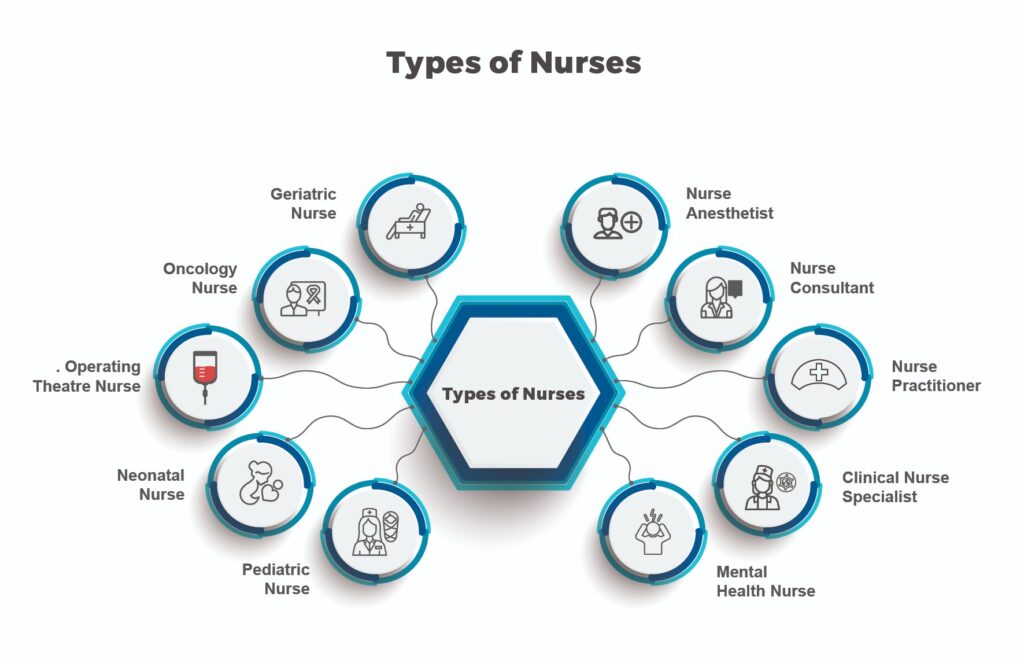
Are you a registered nurse dreaming of adventure, flexibility, and a fatter paycheck? High-paying travel nursing jobs and specialized nursing roles could be your ticket to an exciting career that blends financial rewards with personal fulfillment. Whether you want to explore new cities through short-term travel nursing or climb the ladder to top-paying specialties like Nurse Anesthetist, this guide has you covered. Let’s dive into practical steps to find lucrative opportunities, boost your nurse salary, and build a career you love. image source Why Choose High-Paying Travel Nursing Jobs? Travel nursing jobs are short-term assignments (typically 4-13 weeks) where RNs fill staffing gaps in hospitals, clinics, or other healthcare facilities. These roles are perfect if you crave variety and a competitive income. Here’s why they’re so popular: But not all travel nursing jobs pay equally. To land the highest-paying ones, you need to know where to look and how to position yourself. Plus, if you’re eyeing long-term career growth, specializing in a high-demand field can push your earnings even higher—sometimes over £100,000 a year! What Drives Nurse Salaries? Whether you’re pursuing travel nursing or a specialized role, several factors influence your earning potential: Understanding these factors helps you target the best opportunities, whether you’re staying local or going global. Top 5 Highest-Paying Nursing Specialties If you’re considering a long-term career boost, specializing can significantly increase your income. Based on UK data, here are five of the highest-paying nursing specialties: These roles often require advanced education, but the investment can pay off with higher salaries and job satisfaction. 6 Steps to Find High-Paying Travel Nursing Jobs Ready to hit the road and cash in? Follow these steps to land short-term travel nursing jobs with top pay: Boost Your Career with Education and Certifications To unlock the highest-paying nursing jobs—travel or otherwise—invest in your education. A Master’s in Nursing (MSN) or Doctor of Nursing Practice (DNP) can qualify you for roles like Nurse Practitioner or Nurse Anesthetist. Certifications in specialties like oncology or neonatal care also make you more competitive. Continuous professional development keeps you ahead of trends. Attend workshops, join organizations like the Royal College of Nursing, or take online courses on platforms like Coursera. Staying updated on tech-driven roles (e.g., telehealth) can position you for emerging high-paying opportunities. Going Global: International Nursing Opportunities Want to earn even more? Consider international travel nursing. Countries like the US, Canada, and Australia offer salaries up to £100,000+ for experienced nurses. For example, US Nurse Anesthetists often earn over £100,000, compared to £30,000–£60,000 for similar UK roles. However, weigh the pros and cons: Research credentialing requirements and connect with agencies specializing in international placements to ease the transition. Balancing Pay with Work-Life Harmony High pay is great, but don’t overlook work-life balance. Travel nursing offers flexibility, but crisis roles can be demanding. For less stress, consider specialties like Nurse Educator or Clinical Research Nurse, which offer competitive pay (up to £60,000) with more predictable hours. Roles in outpatient clinics or community health settings also provide a calmer work environment. Take the Next Step Today High-paying travel nursing jobs and specialized roles offer the best of both worlds: financial rewards and a fulfilling career. Start by partnering with a trusted agency, networking with other nurses, and investing in certifications. Whether you’re exploring short-term assignments in new cities or aiming for a Band 9 role in the NHS, the right strategy can help you achieve your goals. Ready to boost your nurse salary and live your dream career? Explore opportunities on NHS Jobs or contact agencies like Pulse Nursing to find your perfect role today!
Per Diem Nursing Jobs: Skills, Benefits, and Top Roles
Looking for a nursing gig that fits your life? Per diem nursing jobs might be your answer. These flexible, high-paying roles let you work when and where you want, no strings attached. Whether you’re a seasoned RN or just exploring options, here’s everything you need to know about per diem nursing—and why it’s shaking up healthcare in 2025. What Are Per Diem Nursing Jobs and Why They Matter? Hey there, nurses and healthcare heroes! If you’re tired of rigid schedules and craving a gig that fits your life, per diem nursing jobs are calling your name. These aren’t just any jobs—they’re short-term, daily shifts where you swoop in to save the day at hospitals or clinics facing staff shortages, busy seasons, or sudden gaps. Think of it as healthcare’s secret weapon: you get paid well, pick your hours, and keep patient care rolling smoothly. Why do they matter? Because they give you freedom and keep facilities running—talk about a win-win! Ready to dive into this game-changer? Let’s explore what makes per diem nursing your next big move. How Per Diem Nursing Works Per diem nursing means working “per day”—you step in when healthcare facilities need extra hands, like hospitals or clinics. You share your available days with a scheduler or agency, and they book you for shifts, sometimes even hours before one starts due to a last-minute call-off. Your role depends on your skills and the facility’s needs—could be a single day or a few. It’s a flexible gig that fits your life, whether you’re easing out of full-time work, juggling family duties, or just craving control over your hours. Demand’s high, and you get to pick when you jump in. Simple, right? Per Diem Nursing vs. Other Nursing Roles Per Diem vs. PRN Nursing Wondering how per diem nursing stacks up against PRN? Let’s break it down. Per diem nurses enjoy the freedom to work across multiple facilities, picking shifts that fit their life—no minimum hours required. PRN nurses, on the other hand, stick to one place, filling in “as needed” with a steadier gig that often includes benefits. The trade-off? Per diem offers flexibility but no guaranteed shifts, while PRN trades some freedom for stability. Which suits you—variety or security? It’s your call! Per Diem vs. Travel Nursing Per diem nursing keeps you close to home, picking shifts in your area, while travel nursing sends you on adventures far away for weeks or months. Both offer flexibility, but per diem skips the suitcase—perfect if you love staying local, whereas travel nursing suits explorers chasing new horizons. Key Skills for Success in Per Diem Nursing Thrive as a per diem nurse with these powerhouse skills! Adapt quickly to new units—every shift feels fresh, and you shine in the challenge. Communicate clearly with teams you’ve just met; it builds trust fast. Work solo with confidence, owning every task like a pro. Embrace the fast pace—it’s your fuel to excel. You’ve got this; these skills turn every new day into your stage to rock! Pros and Cons of Per Diem Nursing Per diem nursing offers flexibility and higher pay, but it also comes with unpredictability. If you’re considering this career path, here’s a balanced look at its advantages and challenges. Pros of Per Diem Nursing ✅ Flexible Scheduling: Work when you want, allowing time for personal commitments or side gigs. ✅ Higher Pay: Per diem nurses often earn more per hour than full-time staff. ✅ Diverse Experience: Exposure to different facilities and specialties helps build skills and prevent burnout. ✅ Career Exploration: Try various roles to find the best fit for your long-term goals. ✅ Networking Opportunities: Work in multiple settings, making connections that could open doors to future jobs. Cons of Per Diem Nursing ❌ Inconsistent Work: Shifts may be available last minute or not at all, making income unpredictable. ❌ No Employee Benefits: Health insurance, paid time off, and retirement plans are typically not included. ❌ Constant Adaptation: Frequent transitions require quick learning of new policies and procedures. ❌ Limited Support: Less access to training and fewer workplace relationships can make it challenging to navigate new environments. Benefits of Per Diem Nursing Jobs Per diem nursing offers unmatched flexibility, allowing nurses to choose when and where they work. They have the freedom to accept or decline shifts based on their availability, making it easier to balance personal responsibilities. Working holidays can bring higher pay, and per diem nurses often earn more than regular staff due to the nature of their role. Without a fixed schedule, they can prioritize family needs while maintaining a rewarding career. How to Become a Per Diem Nurse? Per diem nursing offers flexibility, independence, and variety, making it a great career choice for nurses seeking control over their schedules. Follow these steps to transition into a per diem role successfully: 1. Get Licensed and Certified Complete a state-approved nursing program and pass the NCLEX-RN or NCLEX-PN exam. Depending on your specialty, certifications like ACLS or PALS may be required. 2. Build Clinical Experience Work in different healthcare settings to strengthen your skills. Hospitals, clinics, and home health agencies provide valuable experience that boosts your job prospects. 3. Find Job Opportunities Leverage online job boards, staffing agencies, and professional connections to discover open per diem positions. Networking can lead to better opportunities. 4. Optimize Your Resume Highlight your adaptability, clinical expertise, and ability to thrive in fast-paced environments. A strong resume sets you apart from other candidates. 5. Prepare for Interviews Showcase your ability to work independently, handle changing schedules, and deliver quality patient care. Confidence and preparation make a strong impression. 6. Review and Negotiate Offers Understand pay rates, shift expectations, and benefits before accepting a role. Clarify terms to ensure a good fit. 7. Stay Certified and Informed Keep your license and certifications up to date. Continuous learning enhances your skills and keeps you competitive in the job market. By following these steps, you can successfully launch your per diem nursing career while… Continue reading Per Diem Nursing Jobs: Skills, Benefits, and Top Roles
Amble Medical Services: Expert Healthcare Staffing Solutions
Effective healthcare staffing is crucial for delivering high-quality patient care and ensuring the smooth operation of medical facilities. By implementing appropriate staffing solutions, healthcare organizations can enhance patient satisfaction, reduce staff fatigue, and improve overall efficiency. Comprehensive Healthcare Staffing Solutions At Amble Medical Services, we offer a range of staffing options to meet the diverse needs of healthcare providers: Temporary Staffing Solutions: Ideal for covering short-term vacancies, managing seasonal demands, or addressing unexpected staff shortages Permanent Staffing Solutions: Focused on finding the right long-term fit for your organization, ensuring stability and continuity in patient care. Temp-to-Hire & On-Call Staffing: Provides the flexibility to evaluate staff performance before making permanent hiring decisions, along with on-call support to manage immediate staffing needs. Specialized Healthcare Staffing Services We understand that different healthcare settings require specialized skills. Our services include: Why Choose Amble Medical Services Our commitment to excellence makes us a preferred partner for healthcare staffing: Staffing Solutions for Employers and Job Seekers We serve both healthcare employers and professionals seeking career opportunities: Consulting and Managed Service Provider (MSP) Solutions Beyond staffing, we offer strategic services to optimize your workforce: Why Outsource Your Healthcare Staffing Needs? Partnering with industry experts like Amble Medical Services offers several advantages: Empowering the Future of Healthcare Staffing By choosing Amble Medical Services, you’re investing in quality patient care and building a lasting partnership with a trusted staffing provider. Our expertise and dedication ensure that your facility is equipped to meet current challenges and future demands. Conclusion Effective healthcare staffing is essential for optimal patient outcomes and operational efficiency. Amble Medical Services is committed to providing comprehensive, tailored staffing solutions to meet the unique needs of healthcare providers and professionals. Contact us today to learn how we can support your staffing requirements.
The Shortage of Healthcare Workers in the U.S.
Introduction: In the intricate dance of life, healthcare professionals are the choreographers, ensuring the well-being of individuals and communities. However, the United States faces a formidable challenge: a critical shortage of healthcare workers that imperils the delicate balance of public health. In this article, we embark on a journey to understand the gravity of this shortage, emphasizing the pivotal role healthcare professionals play and unveiling the key factors steering us towards this crisis. Definition of Public Health: The multidisciplinary field of public health is committed to methodically enhancing and preserving the general public’s health. It includes several programs, including community involvement, policy creation, surveillance, health promotion, and disease prevention. Public health professionals seek to determine and treat the root causes of health disorders to create environments that support well-being and halt the spread of disease. Importance of Public Health in Mitigating Healthcare Worker Shortages: Why Is There a Shortage of Healthcare Workers? The problem has recently become especially acute due to the ageing population, including the so-called Baby Boomer generation. This group frequently needs extra medical attention, frequently from professionals in medicine. Those who reach retirement age will require healthcare longer than previous generations because medical advancements have also resulted in individuals having longer lives overall and managing more chronic ailments as they age. There is an increasing shortage of general practitioners to care for the remainder of the population, partly because of this requirement for additional gerontologists and other specialists. It is projected by the American Association of Medical Colleges (AAMC) that by 2032, there will be a 122,000 physician shortfall. The study also predicted that by 2032, the number of people over 65 would have increased by 48%. Regretfully, many practising doctors and the remaining Baby Boomers will soon be prepared to retire. Due to the physician scarcity, rural communities may face more issues than urban ones. The most remote areas, including Guam and the Northern Mariana Islands, as well as rural states like Utah, Vermont, and Tennessee, have the worst shortages of medical professionals per population, according to data for Healthcare Professional Shortage Areas (HPSAs). Where Is the Most Severe Scarcity of Medical Professionals? There are shortages or anticipated shortages in the healthcare sector as the need for qualified healthcare workers rises. Nonetheless, certain occupations have more pronounced labour shortages than others. The shortages are among the most pressing problems facing the contemporary healthcare sector. In 2032, the AAMC predicts a sharp scarcity of doctors. Now, when you consider the specializations of physicians, this scarcity becomes much more significant. Instead of doing family practice or primary care after graduating from medical school, more doctors opt to work in specialized professions. They become specialists by doing a residency and internship in a particular field. Medical school graduates think it is beneficial to pursue these specialities since they are frequently more profitable and prestigious than general medicine. The most significant demand for qualified individuals in this field is in primary care physicians practising general internal medicine, as they are the ones who see the most significant number of patients. One way to address this issue is for healthcare providers to assign certified nurses or physician assistants to fill in for general practitioner physicians. Nurse practitioners and physician assistants can fulfil some of the responsibilities of a general practitioner doctor. They might be required by state law to work under a doctor’s supervision, but the doctor can also manage a team of healthcare providers. Physician assistants and nurse practitioners have lower educational requirements than physicians despite needing a master’s degree and supervised clinical experience. Additionally, nurse practitioners may start with a lower degree and acquire more credentials over time. In the upcoming ten years, the Bureau of Labor Statistics projects that the demand for competent nurses will rise more quickly than the requirement for all other professionals. This rise particularly applies to nurses with a Bachelor of Science in Nursing (BSN). According to estimates cited by the American Association of Colleges of Nursing (AACN), until 2026, the U.S. will require more than 200,000 new nurses per year to replace retiring nurses and fill open posts. Even if more people are enrolling in nursing schools, more is still required to meet demand. Particularly acute shortages exist in fields like education and family nurse practitioners, who are qualified to offer primary care under the direct supervision of a physician. Healthcare organizations may employ travel nurses at several clinics or hospitals to cover brief shortages. Some nurses leave primary care, where there is the greatest need, to work in specialist fields. There is a severe scarcity of forensic nurses, which causes backlogs that impede investigations into crimes like rape and abuse. Family medicine and general practice are also facing a shortage of these nurses. There is a need for more educators as well as nurses. A lack of nursing professors may force certain schools to impose enrollment restrictions. More people aspire to be nurses, but the demand for teachers must be met. According to the AACN, nearly two-thirds of nursing programs turned away competent applicants due to a lack of faculty to instruct them, contributing to the nurse shortages. Nursing homes must also instruct students pursuing associate’s or bachelor’s degrees. Health aides and nursing assistants also require training. Additionally, because there is a need for nurse practitioners, academic institutions require faculty members who can supervise clinical practice for aspiring nurse practitioners and teach in master’s degree programs. Nurses wishing to help close the provider gap by training the next nurse workforce must earn a nurse educator certification before teaching. The United States also needs additional midwives to offer adequate care during childbirth. The lack of O.B./GYNs and problems like the very high rate of cesarean sections in the United States can be handled by midwives. In the United States, midwives attend a mere 8% of deliveries. With a master’s degree and two years of clinical experience, they can offer care during and after childbirth. It is less expensive to give birth under… Continue reading The Shortage of Healthcare Workers in the U.S.
what are the 4 main health care sectors
Introduction: In healthcare, a nuanced comprehension of its diverse sectors is not merely an academic pursuit but a fundamental necessity. This concise overview seeks to elucidate the profound importance of understanding healthcare sectors, offering insights into these components’ pivotal roles in the intricate tapestry of public health. The healthcare landscape is multifaceted, comprised of distinct sectors such as hospitals, pharmaceuticals, health insurance, and medical supplies. Each industry operates as a cog in the healthcare machinery, contributing uniquely to the delivery of medical services, formulation of policies, and the overall well-being of individuals and communities. The imperative to grasp the intricacies of healthcare sectors lies in the far-reaching implications of their functions. Beyond the surface, understanding these sectors unveils their collective impact on public health outcomes, the quality of healthcare services, and the broader socio-economic fabric. This overview is more than a cursory glance; it is an invitation to delve into the intricate dynamics of healthcare sectors. We empower individuals to traverse the complex healthcare landscape with awareness and educated decision-making by peeling back the layers of their operations. Let us explore the significance of understanding the healthcare sector. In doing so, we aim to bridge the gap between the industry’s scientific complexities and individuals’ lived experiences, the knowledge that, at its core, healthcare is a human endeavour with far-reaching effects for all of us. Definition of Healthcare Sectors: Healthcare sectors are specialized sections of the more significant healthcare industry, each providing a specific purpose in delivering, managing, and supporting healthcare services. These sectors work together to provide a comprehensive network that meets the different requirements of individuals and communities seeking medical treatment. Explanation and Significance of Healthcare Sectors Hospitals and clinics provide medical services, including diagnosis, treatment, and care. Significance: They are crucial in offering various medical services, from emergency care to specialized treatments, contributing to community health. This sector researches, develops, and produces research, develops, and produces pharmaceuticals and biotechnological innovations. Significance: It is essential for creating medications, vaccines, and therapeutic solutions, advancing medical treatments and enhancing overall health outcomes. Health insurance involves organizations that provide financial coverage for medical expenses. Significance: It ensures financial access to healthcare services, shielding individuals from the exorbitant costs of medical care. This sector is involved in the manufacturing and distributing of medical equipment, devices, and supplies. Significance: It supports healthcare delivery by providing essential tools for diagnosis, treatment, and patient care, contributing to the effectiveness of medical practices. The Overall Significance Understanding healthcare sectors is vital for several reasons Holistic Healthcare Delivery: Each sector contributes to a comprehensive healthcare system, ensuring that individuals receive various services for their medical needs. Resource Allocation: Healthcare professionals and policymakers can strategically allocate resources, optimizing the efficiency and effectiveness of healthcare services. Policy Development: Insight into healthcare sectors informs the development of policies that address specific challenges, promoting accessibility, quality, and safety in healthcare. Innovation and Progress: Knowledge of healthcare sectors fosters innovation, driving advancements in medical technologies and treatment modalities, ultimately improving healthcare outcomes. In essence, healthcare sectors are integral components of a well-functioning healthcare system, working collaboratively to meet the diverse healthcare needs of society. Top 10 Challenges Healthcare Companies As a result, we must acknowledge the problems posed by digital change in healthcare. This list of healthcare providers’ top ten obstacles will be helpful. Today’s healthcare business challenges are as follows: Electronic health records (EHRs) were introduced to improve patient care and communication and streamline healthcare processes. However, the reality is that many healthcare workers need help adapting to and efficiently using EHR systems. Some critical problems related to healthcare implementation challenges include: Time and Documentation Burden: Physicians frequently spend considerable time documenting patient interactions in EHRs, which can result in higher administrative loads and less face-to-face patient interaction. To support most IT projects, most healthcare organizations have either built their own infrastructure or hired external software development firms, and we are seeing more and more off-the-shelf software supporting the trend. Administrative data, patient medical records, connected device data, transcripts and clinical notes, and patient surveys are all examples of data. However, to manage data received from many sources, most care providers, including top healthcare firms, require more advanced architecture and data management systems. The issue is that relational databases must be more capable of managing unstructured data acquired from many sources, implying that the value of the information they receive is not absolute. Moving from a relational to a non-relational database could assist healthcare practitioners in managing vast amounts of unstructured data. As the business expands and the volume of data increases, the database design can be scaled to accommodate the additional data. To enable integrated health systems, healthcare organizations must prepare all models for all operational, tactical, and strategic management layers and collaborate with reputable integrators. Malicious hackers are drawn to healthcare providers by connected medical devices and a rising desire to retain patient information records. As can be seen, healthcare data breach statistics show increased data breaches from 2009 to 2023. Healthcare firms are moving forward with digitization initiatives due to the impact of technology in healthcare. However, they must exercise extreme caution and implement appropriate safeguards to ensure healthcare cybersecurity, such as: They outsource their IT processes to health technology companies, including sensitive information such as patients’ personal or transactional details. In that situation, companies should only use a third-party source that is HITRUST-certified. As a result, healthcare providers must collaborate solely with reputable software development businesses to address the difficulties of digital transformation in healthcare and manage critical data. The healthcare expense crisis is not new. Many parties, ranging from device makers to medical medication manufacturing businesses and payers to insurance policy providers, play an essential role in setting the cost of healthcare services. When there are so many stakeholders engaged, conflict is unavoidable. Developing a consensus takes time and careful strategy. The rising cost of healthcare directly impacts healthcare organizations’ revenue, as increased costs discourage patients in various ways, from performing lab testing to doing regular… Continue reading what are the 4 main health care sectors